
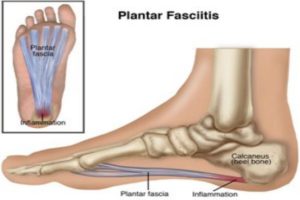
Plantar fasciitis, a musculoskeletal pathology of the foot, is one of the most commonly treated causes of heel pain, occurring in >10% of the American population over their lifetime. The plantar fascia is a thick band of tissue connecting the heel to the ball of the foot, providing support for the arch. Plantar fasciitis refers to inflammation of this band of tissue. Common symptoms include pain at the heel and along the arch or at the ball of the foot when weight is placed on it, especially first thing in the morning or after long periods of rest.
You may also notice symptoms after prolonged periods of standing, when walking barefoot over hard surfaces, or in shoes with poor support. Symptoms tend to decrease as the body warms up, but can become aggravated towards the end of the day or after a long workout. Plantar fasciitis can affect both athletes and non-athletes of all ages who see a sudden increase in activity or increase in body weight.
Physical therapy professionals are trained to evaluate and treat plantar fasciitis in order to help patients return to their favorite activities pain-fee. Patients typically respond well to common rehabilitation approaches such as selective stretching of the calf and foot musculature and strengthening aimed at the hip and ankle. Surgery is always a last resort! For patients who report their most severe symptoms with the first few steps in the morning, stretching before getting out of bed is recommended. Upon awakening, the patient can stretch their plantar fascia by placing a towel around the balls of the foot and toes and pulling the foot towards their body into dorsiflexion.
I also encourage patients to keep a tennis or lacrosse ball at their bedside or in their desk at work to roll on the bottom, or plantar surface, of their feet in a seated position for several minutes. A decrease in calf flexibility is commonly seen in patients suffering from plantar fasciitis due to the gastrocnemius muscle’s attachment at the heel. It is recommended that patients perform a calf or “runner’s stretch” against a wall before taking their first few steps, multiple times throughout the day, focusing on holding the stretch for 30 seconds.
Alternative therapies such as trigger point dry needling performed by one of our specially-trained physical therapists, is effective in treating muscular tension and spasms and can help patients find relief from plantar fasciitis. A therapist will insert small, monomilament needles into the center of the muscle at the site of the “knot” or into the inflamed tendon in order to release tension and promote the healing response.
Dry needling is helpful in decreasing muscle contraction, chemical irritation and improving flexibility. This can be performed on the gastrocnemius and soleus muscles of the calf, the ones often responsible for the decrease in calf flexibility. It also can be used by physical therapists to treat other areas of the body, such as the low back or hip musculature, in order to promote good muscular contraction and prevent compensative patterns responsible for faulty foot biomechanics. A combination of dry needling, soft-tissue mobilization, stretching and strengthening produces the most profound treatment of plantar fasciitis. Ice is also effective at reducing inflammation and generalized foot soreness.
Plantar fasciitis is caused by more than just inflammation in the foot. As a physical therapist, my main focus is finding the root of my patients’ dysfunction. Joint hypomobility, tissue restrictions and muscle imbalances can develop in many parts of the hips, legs and ankles/feet. These dysfunctions compromise the entire body due to the soft tissue’s inability to move freely. All of the body’s processes need to be addressed in order to fully recover from plantar fasciitis.
If you have questions about plantar fasciitis treatments or would like to speak with a physical therapy expert, please contact The Center for Physical Therapy and Sports Medicine.
If you have ever experienced heel or arch pain when you put weight on you foot, particularly when taking your first steps in the morning or after bouts of prolonged sitting, you have most likely had a brush with plantar fasciitis.
The plantar fascia is a thick band of connective tissue which supports the arch on the bottom of the foot. It runs from the heel to the toes and becomes taut whenever the foot is planted (standing, walking, running). It can become inflamed when repeated weight-bearing activity puts a strain on these connective tissues.
Plantar fasciitis is the medical term for inflammation of the plantar fascia. It is an extremely painful and debilitating condition with each episode typically lasting longer than 6 months. In the United States alone, this disorder generates up to 2 million physician visits per year, and accounts for roughly 1% of all visits to orthopaedic clinics. Plantar fasciitis is also the most common foot condition treated in physical therapy clinics.
Although this condition is seen in all ages, it is most commonly experienced during middle age and occurs more frequently in an athletic population, such as runners. Females are affected at a slightly higher percentage than males and >90% of cases are treated successfully with conservative care.
Risk Factors
-Loss of ankle dorsiflexion/decreased calf muscle flexibility
– Tendency to have flat feet
-Excessive foot pronation during the gait cycle
-Improper shoe fit
-Rapid increase in length or levels of activity, such as beginning a new running program or changing to a job that requires a lot more standing or walking than originally accustomed to
-Elevated BMI (Body Mass Index > 30)
-Diabetes Mellitus (and/or other metabolic conditions)
Characteristics/Clinical Presentation
-Heel pain with first steps in the morning or after long periods of non-weight bearing.
-Tenderness to the anterior medial or lateral heel.
-Limited dorsiflexion and tight achilles tendon.
-A limp may be present or may have a preference to toe walking.
-Pain is usually worse when barefoot on hard surfaces and with stair climbing.
-Many patients may have had a sudden increase in their activity level prior to the onset of symptoms.
How Can a Physical Therapist Help?
Physical therapists are trained to evaluate and treat plantar fasciitis. When you are diagnosed with plantar fasciitis, your physical therapist will work with you to develop a program to decrease your symptoms that may include:
-Selective stretching activities to improve calf and ankle flexibility.
-Specific strengthening exercises targeting the trunk, hip or leg musculature.
-Deep tissue massage to the calf and foot musculature to include the plantar fascia in the arch of the foot.
–Dry Needling to reduce pain and improve healing.
-Use of a night splint to maintain correct ankle and toe positions.
-Selection of supportive footwear and/or shoe inserts that minimize foot pronation and reduce stress to the plantar fascia.
-Application of ice, phonophoresis (ultrasound + hydrocortisone) or iontophoresis (electricity + dexamethasone) to reduce inflammation.
–Taping of the foot to provide short-term relief.
Can This Injury be Prevented?
Guidelines for the prevention or management of plantar fascia include:
-Choosing shoes with good arch support
-Replacing shoes regularly, so that they provide sufficient support and shock absorption to your feet.
-Use a thick mat if you must stand in one place for much of the day.
-Applying good principles to your exercise program, such as gradually building up the intensity and duration.
-Stretching your calves and feet before and after running/walking.
-Maintain a healthy body weight.

